Registration Form
Lactation Course for Nurses at Rainbow Children’s Hospital
Rainbow Children’s Hospital is conducting a 20 hours certification course for nurses at a part of the Breastfeeding Support Group. To know more about the course, please connect with us at Click here
Protect Breastfeeding- A Shared Social Responsibility

“Breastfeeding should not be seen as only mother’s responsibility. Let’s make breastfeeding as a shared societal responsibility where not only mother but her whole family, community and even work place are thoughtful about it and facilitate her by giving her an enabling environment.”
This is what the theme of World Breastfeeding Week (WBW) 2021, which is celebrated across the globe from 1st -7th August to raise awareness on breastfeeding. Breast milk is the first vaccine, which protects both mother and the child. It’s the most cost effective intervention for the health care system.
How is fathers, grandparents and family can share this responsibility :
- Help with the baby in between feeds and with older children in family, to allow mother to rest or nap.
- Prepare nutritious meals and snacks to help increase her strengths and energy. Do not let the myths lead the diet practices for mother, give her healthy food without restrictions.
- Help with cleaning and other household jobs to decrease her responsibilities.
- If it’s a big joint family, help her making breastfeeding friendly atmosphere and sharing their experiences.
- Offer positivity and encouragement to prevent post partum blues.
How community can share the responsibility :
- Support breastfeeding in public places like malls, railway stations, airports and bus stands.
- Appreciate breastfeeding as a natural process, please do not frown at mother who is nursing in public area, respect and support her.
- We need champions and ambassadors to support breastfeeding- athletes, film stars, and religious leaders to speak openly about breastfeeding.
How work place can share the responsibility :
- Employers can take a lead role in cultivating supportive workplace so that parents can successfully combine breastfeeding and work.
- Scale up work place lactation by providing a separate, well-ventilated room/place to nurse, pump or store the milk. Let them not express/pump milk in car or a toilet.
- Encourage exclusive breastfeeding for 6months by supporting parental leaves.
Support breastfeeding in preterm and low birth weight babies :
- Preterm and low birth weight babies cannot directly breast feed but they can be fed mother’s only milk by encouraging frequent milk expressions.
- If preterm babies need care in hospital, mothers should be provided with separate milk expression room and hospital grade breast pumps for frequent milk expressions.
- At home breast milk can be expressed, stored and transported in cold boxes to hospital.
- Every hospital should encourage breastfeeding support groups and training of their nursing and healthcare professionals in appropriate techniques and science behind breastfeeding.
- Women should support breast milk banks by donating their extra milk. Human milk banks collect breast milk from healthy mother, pasteurize and keep it frozen to provide it to those preterm babies where mother’s own milk is unavailable.
“Breastfeeding is mother’s domain, but if it is supported by fathers, grandparents, extended families, friends and work places, breastfeeding improves. It’s public health issue which needs investment at all levels.”
Importance of Breastfeeding

From the moment you bring your little one into this world, several people will ask you if you are breastfeeding your baby. They will tell you that you have to do it and that it is important. But here's a little secret, most people don't truly know why it is important. The common assumption is that breastfeeding is what all mothers should do. More than making it a blind rule, we want to help you understand the importance of breastfeeding your child.
- 3 in every 5 newborns are not breastfed right in the first hour after their birth.
- When it comes to exclusive breastfeeding till the age of 6 months, only 41% of infants are breastfed across the globe.
- Over 820 000 children could be saved yearly if all children under the age of 23 months were breastfed optimally.
- Every year, around 45% of child deaths are due to malnutrition.
- In the year 2020, across the world, 149 million children under 5 were estimated to be stunted (too short for age), 45 million were estimated to be wasted (too thin for height), and 38.9 million were overweight or obese.
A. Benefits to Infant/Child:

Being a breastfeeding mother is a true superpower. Your body is wonderfully producing all the sustenance that your little one needs to thrive from day one. Breast milk benefits your baby in more ways than one. There are several benefits it has for babies, nutrition is only one of them. Here are a few key benefits.
- It contains everything a baby needs for first 6 months of life.
- Breastmilk is physiological
- Microbiologically and Biochemically superior
- Sweetest milk
- High Lactose content
- Low protein as compared to cow’s milk but made more of whey protein which is easily digestible.
- Low solute load hence gentle on immature infant’s kidney.
- Microbiologically it is sterile and least chance of contamination.
- It protects infants against various infections such as upper respiratory infections including otitis media and gastro-intestinal infections.
- Breast milk comprises immunoglobulins and Secretory IgA which offer surface protection to respiratory and GI tracts.
- It supplies passive immunity.
- It consists Lactoferrin which is bacteriostatic and inhibits E.coli.
- Its elements Peroxidases and Lipases kill bacteria, Bile Salt Stimulated Lipase (BSSL) kills amoeba and giardia, and Para- amino Benzoic acid (PABA) is important in protection against malaria.
- Amino acids, that are present in the breast milk help in the development of the brain.
- The ratio of Cysteine and Methionine is high and that plays a key role CNS development.
- Rich in Taurine: important neurotransmitter and neuromodulator for brain and retina.
- Breastmilk rich in EFA and LCPUFAs
- Arachidonic and Docosa Hexanoic acid (DHA) are important for Neural and visual development- reduces dyslexia and hyperactivity.
- Breastmilk contains growth regulating factors, growth promoting factors and growth modulators like TSH, thyroxine, GHRF, insulin, Somatostatin, Nerve growth factor
- Breastfed children: score higher on cognitive and IQ tests at school age, and also on tests of visual acuity.
- Also exclusively breastfed preterm have shown higher IQ score and lesser neurological sequelaes with better cognitive abilities.
- Lower incidence of sudden infant death syndrome (SIDS)
- Lower risk of the two most common inflammatory bowel diseases (Crohn’s disease, ulcerative colitis)
- Significantly protected against asthma and eczema,
- Lower risk of obesity in childhood and in adolescence
- Good dental hygiene: have fewer cavities and are less likely to require braces.
- Suffer less often from some forms of cancer (e.g., Hodgkin’s disease, childhood leukemia)
- Lower risk of juvenile onset diabetes.
B. Benefits to mother:

Here is a fact that most people don't know - breastfeeding benefits the mother just as much as it benefits the baby. Yes, by breastfeeding, you are not only providing your baby with nutrition and protection, but you are also taking care of yourself. Now do you see why we say that being a breastfeeding mom is a superpower?
- Breastfeeding offers a range of benefits for mothers as well as their children.
- Women who have breastfed are less likely to develop ovarian and premenopausal breast cancers.
- The more months a woman has spent breastfeeding, the greater the beneficial effect.
- Breastfed mother have lower rate of Type 2 Diabetes and high blood pressure.
- Breastfeeding reduces osteoporosis.
- Breastfeeding mothers enjoy a quicker recovery after childbirth, with reduced risk of postpartum bleeding.
- Exclusive breastfeeding may reduce the risk of anemia by delaying the return of the menstrual cycle for 20 to 30 weeks.
- Mothers who breastfeed are more likely to return to their pre-pregnancy weight than mothers who formula feed.
- Breastfeeding reduces the risk for long-term obesity.
- Natural contraception: Exclusive breastfeeding for the first 6 months postpartum, in the absence of menses, is 98 percent effective in preventing pregnancy.
- Breastfeeding mothers are reported to be more confident and less anxious than bottle-feeding mothers.
- Reduces post-partum depression
- Breastfeeding contributes to feelings of attachment between a mother and her child: mother-infant bonding.
C. Benefits to society/ Epidemiological benefits:

Did you know that breastfeeding is a matter of public health? Yes, studies have proven that communities with a higher rate of breastfed babies have better health. There are fewer diseases risk seen in these communities. The overall health of the community is better with just the simple process of breastfeeding.
- Convenient
- Economical
- Safe for environment
- It is estimated that a breastfed child is 14 times less likely to die from diarrhoea, 4 times less likely to die from Respiratory disease and 2.5 times less likely to die from other infections than a non-breastfed infant
KANGAROO MOTHER CARE

A newborn or a baby is held in a way to provide skin to skin contact. This method is called Kangaroo care. The baby is usually naked with just a diaper on and is held upright on a parent’s bare chest. Both mothers and fathers can perform Kangaroo care on their children. It is most commonly used to comfort and heal premature babies while still in the hospital.
What is kangaroo care?
There are numerous benefits of practising Kangaroo care. One of the most important benefits is to build a bonding between the parents and the child. Holding the baby close to the bare skin can create a special experience that can immensely improve your bonding with your child. But it is not just bonding that you and your child gain from Kangaroo care, it also comes with a plethora of medical benefits.
When performing Kangaroo care, your baby will be placed naked on your bare chest. The baby may be made to wear a hat and a diaper. You and the baby can be wrapped together using a blanket, robe or a hospital gown to provide you with both warmth. This position allows skin-to-skin contact between you and your baby. Each session can last anywhere from minutes to a few hours. This position resembles the way a joey rests inside a Kangaroo’s pouch and hence, is known as Kangaroo care.
How did kangaroo care come about?
Kangaroo care was first developed in Bogota, Colombia towards the end of the 1970s. The mortality rate of premature babies was around 70% during this time. Kangaroo care was created in response to the high mortality rates. The mortality rates during this period were attributed to respiratory problems, infection and even lack of attention. Researches realised that the babies who were held close for long periods by their mothers did not just survive but thrived.
Hospitals in the United States began to encourage that parents, either the mother or the father, to give Kangaroo care to provide skin to skin contact to their pre-term babies for many hours every day they spend in the hospital. Kangaroo care also benefits full-term babies and their parents. All parents are encouraged to give their babies skin-to-skin Kangaroo care.
What are the benefits of kangaroo care?
There are numerous benefits of kangaroo care for pre-term babies, full-term babies and the parents. The benefits of kangaroo care to your baby include:
- Stabilizing your baby’s heart rate.
- Improving your baby’s breathing pattern and making the breathing more regular.
- Improving oxygen saturation levels (this is a sign of how well oxygen is being delivered to all of the infant’s organs and tissues).
- Gaining sleep time.
- Rapid weight gain in your baby.
- Decreasing crying.
- Having successful breastfeeding sessions.
- Leaving the hospital earlier when compared to babies who do not receive Kangaroo care.
The benefits of kangaroo care for parents can include:
- Creating a bonding with your baby and enhancing the feeling of closeness.
- Improving your breast milk supply.
- Improving your confidence in your ability to care for your new baby.
- Creating a sense of control.

Why does kangaroo care work?
Researchers have documented all the benefits of kangaroo care that are listed above in various studies. The studies have found that holding your baby skin-to-skin, can stabilize the baby’s heart and respiratory (breathing) rates. It can also improve oxygen saturation rates, help regulate an infant’s body temperature and lead to the conservation of a baby’s calories. When a mother practices kangaroo care, her baby typically snuggles into her breasts and falls asleep within minutes. The breasts themselves have been known to regulate their temperatures to match your baby’s needs. In other words, your breasts can raise their temperature when your baby’s body is cool and can decrease it when the baby is warm. The extra sleep that your baby had while Kangaroo care is done, assists in regulating body temperature, helps your baby conserve energy and redirect calorie expenditures (use) toward growth and weight gain. The position of the baby on the mother’s breast also helps to stabilise the heart and respiratory rates. It has also been proven that Kangaroo care can have an overall positive impact on the baby’s brain development too.
Common Breastfeeding Conditions

Breastfeeding is not always easy. Every breastfeeding mother suffers from at least one condition that makes the process a little tough. But the rewards of breastfeeding are greater. We would like you to understand the different common conditions seen in breastfeeding women and what can be done to address them.
Fullness of Breasts
- Commonly seen 3-5 days after delivery when breast milk “comes in”
- Breasts feel heavy, hot and hard. Sometimes lumpy
- Milk flows well
Cause- Normal fullness
- Management- Frequent feeds with good attachment
- Resolves after the production of milk adjusts with the baby’s needs
Breasts are swollen, oedematous and skin looks red and shiny
- Affects both breasts diffusely. Painful
- May have fever that subsides in 24 hours
- Nipples become flat and stretched making latching difficult
- Milk does not flow well
Cause
- Delayed initiation of breastfeeding
- Infrequent feeds
- Poor attachment/ineffective suckling
Management
- Milk expression- Manual or Breast pump till the breasts are softer so that baby can attach better
- Frequent feeds
- Pain relief with paracetamol
- Warm compress/ warm shower before expression to allow the milk flow. Cold compress after feeding or expression to relieve congestion
- Breast support
Condition
- A tender localized lump in one breast with redness of skin overlying the lump.
- Untreated, can lead to Mastitis
Cause
- Failure to remove milk from one part of the breast due to poor attachment, tight clothing, trauma to the breast
Management
- Gently massage over the lump before feeding
- Frequent feeding from the affected breast
- Changing position of the baby
Condition
- Hard swelling, redness and severe pain
- Mostly affect only a part of one breast
- Mother has fever and feels sick
- Usually 2-3 weeks postpartum but can occur anytime
Cause - Milk stasis causes non infective inflammation
- Long gaps between feeds ( when mother resumes employment or when baby sleeps through the night)
- Incomplete feeds ( poor attachment/latching)
- Trauma
- Nipple fissure
Management
- Mother should take rest
- Should not stop breastfeeding – start feeding from the unaffected breast to allow the milk let down followed by frequent feeding from the affected breast
- Alternate warm and cold compress to the affected breast
- Analgesics- Paracetamol or ibuprofen
- Antibiotics if no relief in 24 hours
Condition
- Infective Inflammation of breast tissue
- Painful swelling of one breast, full of fluid, skin discoloration, fever
Cause
- Usually secondary to Mastitis which has not been effectively managed
Management
- Drainage of the affected breast (incisional drainage or syringe drainage)
- Antibiotics and analgesics
- Continue feeding from the affected breast
Condition
- Severe pain during suckling.
- Nipple becomes squashed from side to side at the end of a feed
- Visible pressure line at the tip of nipple or at the base
Cause
- poor attachment or poor suckling leading to pulling over the nipple pressing against the hard palate of the baby
Management
- Proper attachment-- almost always instant relief from pain. If latching is poor, break the suction at the beginning and feed after proper latching
- Breast cushions between the feeds to prevent friction.
- Rubbing the breast milk over the nipple and areola at the end of breastfeed prevents soreness and heals the fissure
- Air dry the nipples in between feeds. Avoid using harsh soaps or cleansers
- Feed from the normal breast first, use breast pump or manual expression to empty the affected breast, this allows the nipple to heal and prevent engorgement
Condition
- Symptoms in Mother- Sore nipples with pain continuing between feeds. Pain not relieved by improved attachment
- Red or flaky rash over the areola with itching and depigmentation
- Symptoms in Baby- white spots inside cheeks or over the tongue that cannot be removed easily
- Some babies feel distressed when they try to attach or feed, suggesting a sore mouth
- There may be an associated red rash over the nappy area (Diaper dermatitis)
Cause
- Fungal infection Candida albicans , Often following the use of antibiotics in mother or baby
Management
- Both mother and baby should be treated with Gentian violet paint or Nystatin
Condition
- Flat nipples are protractile- if mother pulls them out, they stretch in the same way as in baby’s mouth
- Inverted nipples are mostly non protractile- does not stretch when pulled and the tip goes in. Makes it difficult to latch.
- Large or long nipple makes it difficult for the baby to take most breast tissue into the mouth
Management
- Milk expression and feeding with cup
- Express milk into the baby's mouth, and touch the lips to stimulate the rooting reflex and encourage the baby to open his or her mouth wider.
- Breast pump to get the milk flowing and pull the nipples out as much as possible before placing baby at the breast for a feed
- Nipple shields are thin, silicone shields that fit over the nipple that help the nipple protrude more, which makes latching easier
- For inverted/ flat nipples, a mother can use a 20 ml syringe, with the adaptor end cut off and the plunger put in backwards to stretch out the nipple just before a feed
Condition
- Breast augmentation, lift and reduction procedures potentially affect nerves and ducts within the breast, thus affecting lactation
- Breast implants below the muscle affect milk production
- The amount of milk made will depend on the number of connected ducts and functionality of the nerves that enable lactation, as well as other factors apart from the surgery, such as hormones and milk expression
- Partial / total mastectomy can reduce the capability to breastfeed or produce breast milk
- A single breast can produce enough breast milk for healthy infant growth.
Management
Prenatal support:
- Talk with mothers who have had breast surgery about the type of surgery, placement of incisions, and underlying reasons for the surgery to understand the potential for reduced milk production.
- Examine mothers’ breasts to identify possible insufficient glandular tissue and provide anticipatory guidance for breastfeeding support.
Postpartum support:
- Closely monitor infants of mothers who have had breast surgery to be sure that the infant receives optimal nutrition for growth.
- When mothers present with insufficient milk production postpartum, inquire about prior breast surgery as part of your assessment.
- Refer to an International Board Certified Lactation Consultant (IBCLC) to teach mothers who have had breast surgery how to stimulate production and/or how to supplement with pasteurized donor human milk or formula
Myths and Facts

Look at the list of myths below. How many of these have you heard? Yes, all of these are myths. Information is aplenty between family, friends and the internet. It is hard to identify what is a myth and what is a fact. While some myths are harmless, some myths can end up being dangerous to you and your baby and your overall experience of breastfeeding. Read through some of the common myths and understand the facts.
Babies are born with the reflex to look for their mother’s breast. Breast feeding a natural process, however many mothers need practical support with positioning their baby for breastfeeding and making sure their baby is correctly attached to the breast. Breastfeeding takes time and practice for both mothers and babies. Breastfeeding is also time intensive, so mothers need space and support at home and work.
Many mothers experience discomfort in the first few days after birth when they are learning to breastfeed. But with the right support with positioning their baby for breastfeeding and making sure their baby is correctly attached to the breast, sore nipples can be avoided. If a mother faces breastfeeding challenges like sore nipples, support from a lactation consultant or other skilled professional can help them overcome the issue.
Washing your nipples before breastfeeding isn’t necessary. When babies are born, they are already very familiar with their own mother’s smells and sounds. The nipples produce a substance that the baby smells and has ‘good bacteria’ that helps to build babies’ own healthy immune system for life.
Doctors, nurses and midwives often encourage the practice of ‘skin-to-skin’ – also known as kangaroo mother care – immediately after birth. Bringing your baby in direct contact, so their skin is against yours, is a very important practice that helps them to find and attach to the breast. If you can practice this within one hour after birth and then frequently after, it helps to establish breastfeeding. If the mother cannot do this, then the partner or another family member can step in. Fact: Simply stated: ‘the more you feed, the more milk you make’.
Like everybody else, breastfeeding mothers need to eat a balanced diet. In general, there is no need to change food habits. Babies are exposed to their mother’s food preferences from the time they are in the womb. If a mother perceives that her baby reacts to a specific food she eats, it is best to consult a specialist.
Exercise is healthy, also for breastfeeding mothers. There is no evidence that it affects the amount and taste of your milk.
It is easier to get breastfeeding started if you begin in the first hour after birth because a baby’s reflexes are very strong at that time. They are ready to learn to feed at the breast. If you do not latch your baby on right after birth, do it as soon as possible in your situation. If you need help putting your baby to the breast, ask for support from a qualified lactation consultant or other skilled professional. Frequent skin-to-skin contact and putting your baby to the breast will help to get breastfeeding going.
Almost all mothers produce the right amount of milk for their babies. Breastmilk production is determined by how well the baby is latched on to the breast, the frequency of breastfeeding and how well the baby is removing milk with each feeding. To keep breastmilk production going, continue offering the breast to your baby as often as possible. Breastfeeding isn’t a ‘one woman’ job and mothers need support. Support like ongoing breastfeeding guidance from health care providers, help at home, and staying healthy by eating and drinking well.
Some of you may not make milk for the first 3 to 5 days after delivery however you make a thick concentrated liquid called Colostrum. This is rich in all the nutrients that are required for the new born baby.
Breast milk is easier to digest than formula milk which is probably why your baby is requiring frequent feeds. Needing a feed every 2 to 3 hours is normal for new born babies.
Studies have shown that even malnourished women are able to produce milk of sufficient quality and quantity to support a growing infant. Most cases low weight gain are related to insufficient milk intake or an underlying health problem in the baby.
Depending on the kind of illness, mothers can usually continue breastfeeding when they’re sick. You need to make sure you get the right treatment, and to rest, eat and drink well. In many cases, the antibodies your body makes to treat your disease or illness will pass on to your baby, building his or her own defences.
It’s important to inform your doctor that you are breastfeeding and to read the instructions with any medications you buy over the counter. It might be necessary to take medications at a specific time or in a specific dosage, or to take an alternative formulation. You should also tell the baby’s doctor about any medications that you’re taking
All babies are different. Some are clingy and some are not, no matter how they are fed. This is an absolute myth however formula fed babies may sleep longer. Breastfeeding provides not only the best nutrition for infants, but is also important for their developing brain. Breastfed babies are held a lot and because of this, breastfeeding has been shown to enhance bonding with their mother.
There’s no evidence that it is more difficult to stop breastfeeding after one year, but there is evidence that breastfeeding up to two years is beneficial for both mothers and children.
Many mothers continue breastfeeding after going back to work. If you have the right to time and a place to breastfeed during working hours, you may be able to go home and breastfeed, ask a family member or friend to bring your baby to you, or to express your milk and take it home. If you decide to give your baby a breastmilk substitute for some feeds, it still very good. to continue breastfeeding whenever you are with your baby
ANATOMY AND PHYSIOLOGY OF LACTATION

Mammary glands are modified sweat glands
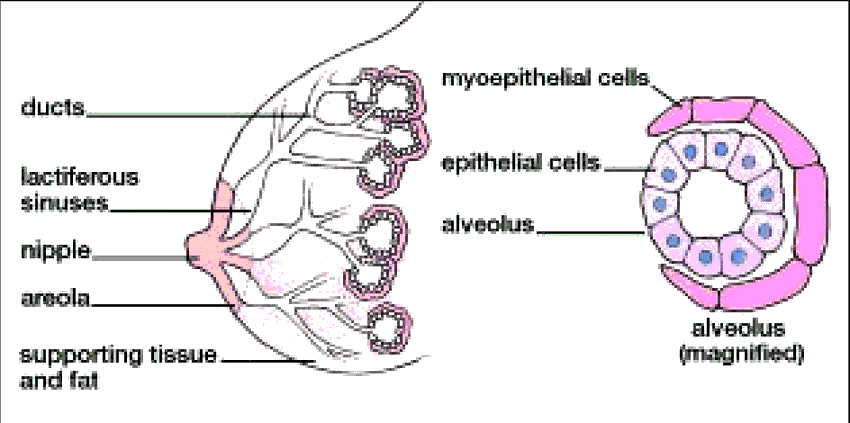
Mammary glands are primarily composed of adipose and collagenous tissue. Mammary glands make up a very minor portion of the total breast volume. The mammary gland is made up of lactiferous ducts that transport milk, which become more expansive and branch extensively during a woman’s pregnancy in response to hormones like estrogen, cortisol, prolactin and growth hormone. In response to progesterone, clusters of breast alveoli grow from the ducts and expand outward toward the wall of the chest. Breast alveoli resemble balloon-like structures and are lined with milk-secreting cuboidal cells called lactocytes. These are surrounded by a net of contractile myoepithelial cells. Milk is secreted from the lactocytes, fills the alveoli, and is then squeezed into the ducts. Clusters of alveoli that drain to a common duct are known as lobules; a lactating female has 12–20 lobules organized in a radial fashion around the nipple. Milk drains from lactiferous ducts into lactiferous sinuses which meet at 4 to 18 perforations in the nipple which are called nipple pores. The small bumps on the areola (the darkened skin around the nipple) are known as Montgomery glands. They secrete oil that helps to cleanse the nipple opening and, prevent cracking and chapping of the nipple during breastfeeding.
Physiology of Lactation
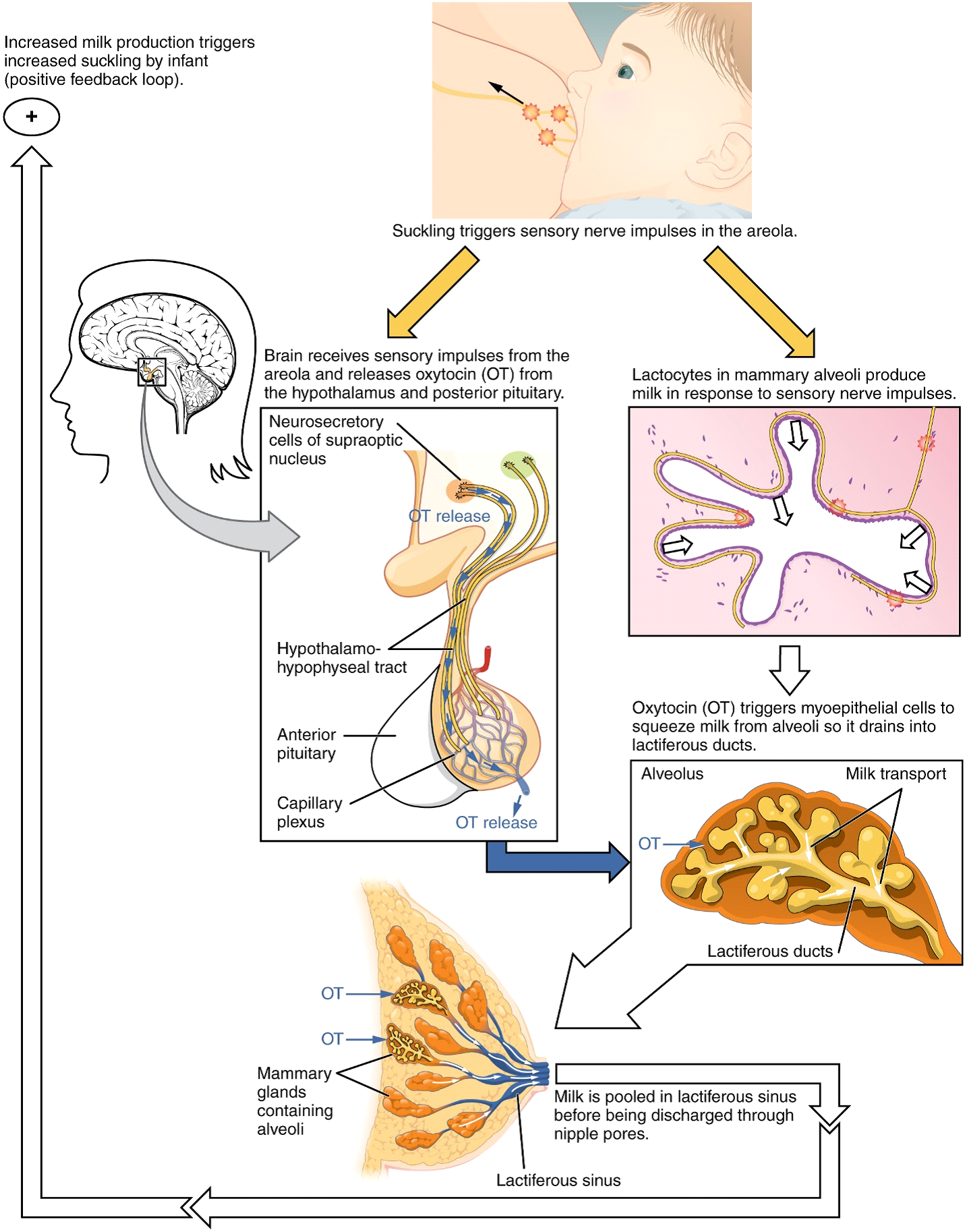
Prolactin, the pituitary hormone plays an important role in the production and maintenance of breast milk supply. It also mobilizes maternal micronutrients to be secreted in the breast milk. By the fifth week of pregnancy, the circulating prolactin level begins to increase. It eventually rises to approximately 10–20 times of the pre-pregnancy concentration. During the progress of pregnancy, prolactin and other pregnancy hormones helps to prepare the breast’s anatomy for the secretion of milk. Prolactin levels plateaus and stabilizes in late pregnancy, and remains at a level high enough to enable milk production. However, placental hormones like estrogen, progesterone inhibit prolactin-mediated milk synthesis when the woman is still pregnant. When the placenta is expelled during delivery, the inhibiting placental hormones withdraw leading to a sudden increase in the levels of prolactin hormone. This in turn helps initiate milk production. After childbirth, there is a sharp drop in the baseline prolactin levels, but its level is restored in a 1-hour spike when breast feeding is done to help stimulate the milk production for the next feeding. With each spike in prolactin level, the levels of estrogen and progesterone also slightly increase. When an infant suckles on the breast, the sensory nerve fibres of the areola trigger a reflex known as neuroendocrine reflex. It signals milk secretion in lactocytes and it is collected in the alveoli. The posterior pituitary releases the hormone oxytocin. Oxytocin stimulates the myoepithelial cells to help squeeze milk that is collected in the alveoli and drains it into the lactiferous ducts. The milk then collects in the lactiferous sinuses, and finally discharges through the nipple pores on the nipples. It takes no longer than 1 minute from when an infant begins the suckling (the latent period) to the secretion of the milk (the let-down).
Stages of Lactation
Mammogenesis: Development of breast tissue, mammary gland, lactiferous tubules. Starts from puberty till early pregnancy
Lactogenesis, stage 1: Mid pregnancy till day 3 post natal. Initiation of milk synthesis in the alveoli.
Lactogenesis, stage 2: Day3 to day 8, Secretion of the milk, due to sudden withdrawal of progesterone and rise of prolactin.
Galactokinesis: Ejection of the milk from the let-down reflex, switch from endocrine control to autocrine control
Galactopoiesis: Maintenance of lactation from day 8 till involution starts
Involution: Cessation of milk, approximately 40 days from the last breastfeeding
Breastfeeding Special Circumstances

The importance of breastfeeding for the mother, the baby and the society needs no emphasis. But there are some unique and special situations where the family, as well as the health care providers, face a dilemma as to what to do with breastfeeding. This brief review highlights the special situations and possible adjustments to breastfeeding.
What are the special situations?
Special situations can be maternal or baby related. They can be medical or non-medical, social situations. Medical situations can be infections, medical problems, surgical interventions, investigations, hospitalisation for various reasons, vaccinations etc. The common baby related situations are twin or triplet gestation, jaundice, prematurity, heart or neurological problems in the baby. The usual social situations are travel, mother returning to work and so on.
Maternal infections:
- It is safe for a mother infected with hepatitis B virus (HBV) to breastfeed her infant. All infants born to HBV-infected mothers should receive hepatitis B immune globulin (HBIG) and the first dose of hepatitis B vaccine within 12 hours of birth.
- HCV infection is not a contraindication to breastfeeding.
- CDC and the AAP advise that HIV-infected mothers should completely avoid breastfeeding their infants. ART and maternal viral load should not be considered in this circumstance. For developing countries - WHO recommends that HIV-infected mothers breastfeed exclusively for the first 6 months of life and continue breastfeeding for at least 12 months, with the addition of complementary foods. These mothers should be given ART to reduce the risk of transmission through breastfeeding.
- Current evidence shows that breast milk is probably not a source of transmission in the case of SARS-C0V-2. A child being breastfed by a COVID-19 positive person should be treated as a person of close contact with COVID-19, and the appropriate quarantine procedures should be followed. Someone who is fully vaccinated against COVID-19 and is not at increased risk for severe illness from COVID-19 can feed EBM to the child.
- A person who is breastfeeding should follow certain precautions when serving their recommended period of isolation: Wash their hands using soap and water before touching their child or expressing breast milk either by hand expression or with a breast pump. If soap and water are not available, use hand sanitiser with at least 60% alcohol. Wear a mask when they are less than 6 feet from the child (including when feeding at the breast or feeding from a bottle) and when expressing breast milk. Clean and sanitize breast pumps and all infant feeding items.
- Breastfeeding mothers with diarrhoea should continue breastfeeding and increase their own fluid intake. Exclusive breastfeeding protects infants against diarrhoea.
- Mothers with herpes simplex can continue to breastfeed if no lesions are present on the breasts and if lesions elsewhere on the body are carefully and fully covered. Mothers with active lesions on the breast should temporarily stop breastfeeding from the affected breast and should not feed expressed breast milk from the affected breast.
- Flu does not spread to infants through breast milk. A mother with suspected or confirmed flu should take all possible precautions to avoid spreading the virus to her infant while continuing to provide breast milk to her infant. Flu vaccination is safe for breastfeeding women.
- Mothers should temporarily NOT breastfeed but CAN feed expressed breast milk if she has untreated, active tuberculosis. The mother may resume breastfeeding once she has been treated appropriately for 2 weeks and is documented to be no longer contagious. Airborne and contact precautions may require temporary separation of the mother and infant, during which time expressed breast milk should be given to the infant by another care provider.
- Mother who has active varicella (chickenpox) infection that developed within the 5 days prior to delivery to the 2 days following delivery should temporarily not breastfeed but can feed expressed breast milk.
Maternal medical conditions:
Mothers with medical conditions like hypothyroidism, diabetes or hypertension can safely continue to breastfeed.
Investigations:
⦁ Breastfeeding should not be interrupted if the mother has an X-ray, MRI, CT, Angiogram, Ultrasound or Mammogram.
⦁ If a breastfeeding mother is having a nuclear medicine scan (eg. bone, VQ, myocardial perfusion or parathyroid scan), breastfeeding and close contact may need to be restricted, depending on the radiopharmaceutical used.
⦁ A mother can express beforehand and give this milk to her baby while she is waiting. During this time she can be encouraged to express and store her breast milk for use after the withholding period, as the milk will also lose its radioactivity in this time.
Maternal medications:
⦁ Most medicines pass into breast milk in very small and weak amounts, so they do not harm the baby. It is usually more harmful to the baby to stop breastfeeding.
⦁ The US National Library of Medicine (NLM) at the National Institutes of Health (NIH) maintains LactMed®, a database containing information on drugs and other chemicals to which breastfeeding mothers may be exposed.
⦁ HCPs should weigh the risks and benefits when prescribing medications to breastfeeding mothers by considering:
⦁ Need for the drug by the mother.
⦁ Potential effects of the drug on milk production.
⦁ Amount of the drug excreted into human milk.
⦁ The extent of oral absorption by the breastfeeding infant.
⦁ Potential adverse effects on the breastfeeding infant.
⦁ Age of the infant.
⦁ The proportion of feedings that are breast milk.
⦁ Yellow Fever (live virus) is contraindicated during lactation
Maternal surgeries:
⦁ Most mothers who have had breast surgery are able to produce some milk. Some surgeries impact milk production more than others.
⦁ Mothers may need support to increase milk production and/or to supplement with pasteurized donor human milk or formula.
Hospitalisation:
⦁ When a mother or her child needs hospital care, breastfeeding should be continued as much as possible unless contraindicated for medical reasons. Whenever possible baby should be kept with the mother.
⦁ Most mothers find that even if their supply does drop while they are in hospital, it soon builds up again when they are home and feeding normally.
⦁ For planned elective admissions, milk can be expressed and stored beforehand
Pregnancy:
If a nursing mother becomes pregnant, she can continue to breastfeed.
Careful consideration has to be given to the nutritional needs of the mother
Multiple gestation:
Twins can be fed simultaneously or with expressed breast milk
Prematurity:
Breast milk is extremely important for a preterm baby. Direct feeding may not be possible initially. EBM should be given. Milk expression must start as soon as possible after the birth of the baby.
Kangaroo mother care and Non-nutritive sucking will be beneficial to establish breastfeeding.
Neonatal jaundice:
⦁ Most newborns with jaundice can continue breastfeeding
⦁ Decisions about supplementation of a jaundiced newborn should be made on a case-by-case basis.
Birth defects:
⦁ Babies with a cleft of the lip only can usually breastfeed as a newborn. Breast or fingers can be used to block the cleft to help the baby to get proper suction.
⦁ Babies with cleft palate - will most likely require some assisted techniques and/or lactation aids.
⦁ Comfort sucking can still be continued
Congenital heart disease or neurological problems:
⦁ Breast and bottle feeding can be difficult for some infants with CHD/ Neurological diseases or genetic syndromes.
⦁ Some babies may also have trouble coordinating their sucking, swallowing and breathing. This may lead to the need for supplementation with either breast milk or formula via nasogastric tubing.
⦁ Expressed breast milk should always be the choice if direct breastfeeding is not possible. Persistence and time will often help
Lactose or milk protein intolerance:
⦁ A baby with symptoms of lactose intolerance should not be taken off the breast and fed on soy-based or special lactose-free infant formula, except in the very rare primary lactose intolerance.
⦁ Cows' milk protein allergy (or intolerance) is often confused with lactose intolerance. Removal from the mother's diet of the foods to which the baby is allergic or intolerant can sometimes help.
Return to work:
⦁ While away from their child, mothers need to express breastmilk at similar intervals that they would normally breastfeed.
⦁ Bottles of expressed breastmilk need to be carefully prepared, stored and warmed.
Travel and breastfeeding:
⦁ Breastfeeding or expressing milk should be continued when travelling.
⦁ If travelling without the baby, breast milk should be expressed in advance so that the child may continue to have milk while the mother is away.
⦁ Babies who have never been fed milk from a bottle or cup should practice with another caregiver.
⦁ If storing and/or shipping breast milk is not possible, “pumping and dumping” can allow maintaining milk supply.
Breastfeeding Positions

While breastfeeding is a natural process, it can be uncomfortable for the mother at first but there is no reason for worry or panic. Breastfeeding is a learning process for both the mother and the baby. There is no position that can be prescribed as the best to feed your baby. The best position is one that is discovered to be most comfortable for both the mother and the baby and is often found after a lot of trial and error. The position chosen for breastfeeding can also change as the baby grows and starts to become more mobile too. Knowing a few basic breastfeeding positions can help you determine which of them work the best for you and the baby.
Cross-Cradle Hold
Sit up in a comfortable chair with your back straight. Cradle your baby crosswise and support the baby with the arm opposite to the breast that you are feeding the baby from. If you are feeding the baby from the left breast, hold the baby in your right arm with the baby’s head in your palm and vice versa. Use your free arm to guide your breast into the baby’s mouth to help it latch on properly. This position is best for early breastfeeding of newborns. Remember not to lean over or bend forward to bring your breast to your baby as it will cause back pain. Instead lift your baby to your breast.
Cradle Hold
This position is similar to the previously mentioned cross-cradle hold with the only difference being in the position of the baby. Here, the baby is held using the arm on the same side as the breast you are using to feed the baby. The head of the baby will now be supported by the crook of the elbow and the palm of the hand will support the body of the baby. The free hand can be used to support the baby or to guide the breast for a better latch. Remember to sit up with your back straight. A pillow can be placed on the lap for extra support.
Football-Hold
The football-hold is a popular position among mothers who have undergone a caesarean birth, have large breast, are nursing two babies at once or are feeding a premature baby. In this position, the baby is held at your side with your elbow bent. The open hand will support the baby’s head and the forearm will support the baby’s back. A pillow can be placed at your side under your arm for support and use chairs with broad and low placed arms.
Side-lying Hold
If you are recovering from a cesarean birth, you may have to be in a reclining position while breastfeeding for the first few days. A lying position can be a great way to rest while your baby feeds and can also be great for a good latch. To feed in the lying down position, lie down on your side facing the baby. Use a hand to guide the nipple to your baby’s mouth. Once a good latch is formed, you can use one arm to support your head and the other to support and comfort the baby.
To receive email releases, simply provide
us with your
email below
Our Contacts
- 1-800-2122
- breastfeedingsupport@rainbowhospitals.in